Gum recession occurs when the soft tissue around the teeth pulls back, exposing the roots. This condition can cause tooth sensitivity, aesthetic concerns, and, if left untreated, even tooth loss. Early diagnosis and the right treatment approach are essential to preserve gum and tooth health. In this article, we will explore both surgical and non-surgical methods used to treat gum recession.
Non-Surgical Treatment Methods
Non-surgical treatments are often effective in the early stages of gum recession or when addressing the underlying causes. The main goal is to stop the progression of the condition and promote healthy gum reattachment.
Professional dental cleaning (scaling): Plaque and tartar buildup are major contributors to gum recession. Regular professional cleanings help reduce inflammation and irritation, supporting overall gum health.
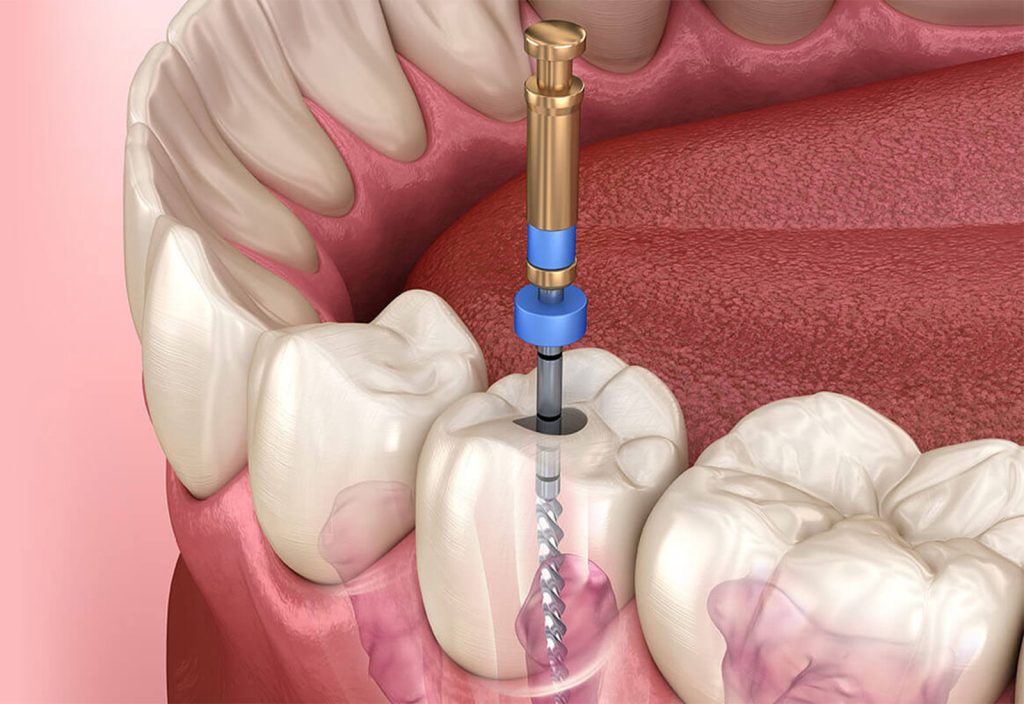
Root planing and curettage: This deep-cleaning procedure removes bacteria and hardened deposits below the gum line. Root planing smooths the tooth roots, while curettage eliminates inflamed gum tissue, encouraging reattachment of healthy tissue.
Improving oral hygiene habits: Using the right toothbrush, practicing correct brushing techniques, and cleaning between teeth with dental floss or interdental brushes are key to halting recession.
Reducing risk factors: Addressing habits such as smoking, teeth grinding (bruxism), and misaligned teeth through lifestyle changes or orthodontic treatment can protect the gums from further damage.
Non-surgical treatments are generally the first step, especially when the recession is mild or caused by reversible factors like inflammation.
Surgical Treatment Methods
When gum recession is more advanced or affects visible areas, surgical treatments may be required. These procedures restore the gum line, protect exposed roots, and improve both function and aesthetics.
Connective tissue graft: Tissue taken from the patient’s palate is placed over the affected area to cover the exposed root. This method strengthens the gum and improves its appearance.
Free gingival graft: Used when there is minimal gum tissue, this technique adds new tissue to widen and reinforce the gum line, preventing further recession.
Lateral flap technique: Healthy gum tissue adjacent to the recessed area is repositioned to cover the exposed root. This method is often preferred for localized cases.
Regenerative techniques: In certain cases, biomaterials or growth factors are applied to stimulate the regeneration of bone and gum tissue.
Surgical methods are chosen only when necessary and based on a detailed dental evaluation. These procedures help rebuild the gum line and reduce the risk of future tooth loss.
Post-Treatment Care and Long-Term Protection
Regardless of the treatment method, the long-term success of gum recession therapy depends heavily on post-treatment care and regular dental visits.
Regular dental checkups: Your dentist should monitor healing and gum stability after treatment.
Consistent oral hygiene: Continue brushing gently with a soft-bristled toothbrush, use proper brushing techniques, and maintain flossing and interdental cleaning routines.
Healthy lifestyle: Balanced nutrition and good overall health support strong gums and faster healing.
Avoiding trauma: Refrain from habits that strain the gums, such as biting hard foods or clenching your teeth.
Following these recommendations helps maintain the treatment results and supports long-term gum health.
Conclusion
The choice between surgical and non-surgical treatment for gum recession depends on the extent, cause, and progression of the condition, as well as the patient’s overall oral health. Non-surgical methods like scaling and root planing are often sufficient in early cases, while advanced recession may require surgical options such as connective tissue grafts or flap procedures. A thorough dental examination is essential to determine the right approach, and ongoing care is crucial for lasting results.
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice. Each patient’s condition may vary. For accurate diagnosis and treatment, consult a qualified dentist or periodontist.